An Orthopedic information source updated by the physicians of Cooley-Dickinson Medical Group Orthopedics and Sports Medicine; aimed at helping the active population of Western Massachusetts get the most out of life.
Saturday, December 26, 2015
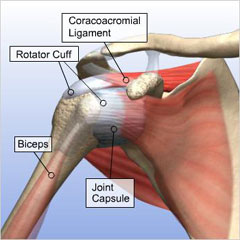
How Do We Repair the Rotator Cuff?
Rotator cuff tears are a very common problem in the older, active population. If you are like most people, you know someone that has been through shoulder surgery to repair the torn tendons but do you know how it was done? Check out this animation from the American Orthopedic Society of Sports Medicine that explains the principles behind repairing a rotator cuff tear.
Monday, December 14, 2015
A Body in Motion...
Newton's First Law:
"When viewed in an inertial reference frame, an object either remains at rest or continues to move at a constant velocity, unless acted upon by an external force."

While Sir Isacc Newton was describing inanimate objects, this law is also true of humans and more topically, joints. With age and stress, the joints of our body break down. This process is often referred to as the Osteoarthritis, or more generically Arthritis. As joints become painful and inflamed, we move them less and they get stiffer. Along with the joints getting stiffer, the muscles weaken from disuse. The tendons become unhealthy and fragile and the ligaments tighten our joints even further. All of these processes conspire to "remain at rest". One of the mainstays of initial treatment for arthritis is physical therapy. The goal is to stem the tide of these degenerative processes with the hope of keeping us moving at a "constant velocity". While physical therapy is wonderful, it is not for everybody. There can be an expensive co-pay, the therapist's hours may not fit your life and the frequently traditional approach to disease and the human body may not fit your personality. Fortunately, there are alternatives! In a recent national meeting of the American College of Rheumatology, a series of studies were presented demonstrating the benefits of Tai Chi.
In a nicely done study, they found that a twice a week session with Tai Chi instruction was at least as good, if not better for patients with Osteoarthritis of the knees. It should be no surprise that a low impact exercise regimen that focuses on balance and strength, and includes life affirming meditation would be useful for people with knee arthritis. It has been demonstrated in the past to be useful in preventing hip fractures when use regularly in the elderly population. From these results, one could easily extrapolate that the practice of Tai Chi, or something similar would be good for people with arthritis of really any joint within the body.
There are many ways to say it: "Motion is Lotion", "People are like sharks, if they don't move, they die.", "Move it or Lose it!". The basic notion is the same, do what Newton recommends and stay in motion.
"When viewed in an inertial reference frame, an object either remains at rest or continues to move at a constant velocity, unless acted upon by an external force."

While Sir Isacc Newton was describing inanimate objects, this law is also true of humans and more topically, joints. With age and stress, the joints of our body break down. This process is often referred to as the Osteoarthritis, or more generically Arthritis. As joints become painful and inflamed, we move them less and they get stiffer. Along with the joints getting stiffer, the muscles weaken from disuse. The tendons become unhealthy and fragile and the ligaments tighten our joints even further. All of these processes conspire to "remain at rest". One of the mainstays of initial treatment for arthritis is physical therapy. The goal is to stem the tide of these degenerative processes with the hope of keeping us moving at a "constant velocity". While physical therapy is wonderful, it is not for everybody. There can be an expensive co-pay, the therapist's hours may not fit your life and the frequently traditional approach to disease and the human body may not fit your personality. Fortunately, there are alternatives! In a recent national meeting of the American College of Rheumatology, a series of studies were presented demonstrating the benefits of Tai Chi.
In a nicely done study, they found that a twice a week session with Tai Chi instruction was at least as good, if not better for patients with Osteoarthritis of the knees. It should be no surprise that a low impact exercise regimen that focuses on balance and strength, and includes life affirming meditation would be useful for people with knee arthritis. It has been demonstrated in the past to be useful in preventing hip fractures when use regularly in the elderly population. From these results, one could easily extrapolate that the practice of Tai Chi, or something similar would be good for people with arthritis of really any joint within the body.
There are many ways to say it: "Motion is Lotion", "People are like sharks, if they don't move, they die.", "Move it or Lose it!". The basic notion is the same, do what Newton recommends and stay in motion.
Sunday, November 1, 2015
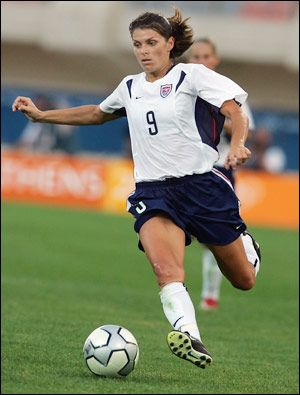
How Safe is Artificial Turf?
There is a well intentioned women's soccer coach from the University of Washington who has brought up the possibility that the new generation of artificial turf is causing cancer in young athletes. The first generations of artificial turf (AstroTurf) were thought to cause too many injuries in the athletes. These surfaces were painful to play on and brought on a host of new injuries (rug burn, turf toe, etc...). Enter the new generation of artificial turf, a combination of subsurface of stone and recycled rubber covered by artifical blades of grass and an in-fill of crumb rubber made from old tires. These new surfaces decrease landfill use by re-using old tires. They significantly decrease the use of water and fertilizer. They decrease the maintenance costs. But are they safe? Athletes will spend countless hours sliding, diving and rolling around on these fields. They will come home with black rubber granules embedded in their elbows, knees and shins. They will end up with them in their ears, nose and mouth. Along with Coach Griffin, there are a number of watchdog groups that have continued to advocate for young athletes by questioning if chemicals released by the re-purposed rubber is causing cancer.
The publicity was bad enough that a principal of a Maine elementary school wrote to the company that installed the Rubercycle surface at her school. The school was searching for data to make an informed decision on weather to remove the existing playground surface. The response she received was not from the company but from a Toxicologist from MIT and an environmental risk assessment firm. Attached is her thorough and thoughtful review of the current research, leading her to the conclusion:
"... I have examined the relevant evidence, and have found that rubber mulch is neither known nor reasonably expected to cause cancer, and is otherwise safe for use in playgrounds. I know of no reason that this mulch should be removed from the playground at Jonesport Elementary School."
This response was fairly convincing and consistent with any scientific evidence that I have read. If you want more information on the subject, the Synthetic Turf Council summarizes a number of the recent research efforts.
The publicity was bad enough that a principal of a Maine elementary school wrote to the company that installed the Rubercycle surface at her school. The school was searching for data to make an informed decision on weather to remove the existing playground surface. The response she received was not from the company but from a Toxicologist from MIT and an environmental risk assessment firm. Attached is her thorough and thoughtful review of the current research, leading her to the conclusion:
"... I have examined the relevant evidence, and have found that rubber mulch is neither known nor reasonably expected to cause cancer, and is otherwise safe for use in playgrounds. I know of no reason that this mulch should be removed from the playground at Jonesport Elementary School."
This response was fairly convincing and consistent with any scientific evidence that I have read. If you want more information on the subject, the Synthetic Turf Council summarizes a number of the recent research efforts.
Wednesday, October 7, 2015
Readers Choice Award
We are excited to announce that our orthopedic group has been chosen for the Gazette Readers Choice award. Congratulations and thank you to all of the staff and doctors that have helped us take care of so many people. Keep up the great work!
Monday, July 20, 2015
Coaches can be a strong influence in preventing football injuries, say researchers | EurekAlert! Science News
Coaches can be a strong influence in preventing football injuries, say researchers | EurekAlert! Science News
This is exactly why programs such as the Northampton Cal Ripken League are so important. Programs that coach the Coaches are critical for youth sports and vital for our kids.
Friday, July 10, 2015
Achilles Tendon Injuries
Achilles tendon and calf muscle tears are problems that have recently become near and dear to my heart. This, much like tennis elbow is the source of many athletic midlife crises. The Achilles tendon is actually a combination of three separate tendons. The Gastrocnemius is the big, bulbous muscle that gives the calf muscle shape. The Soleus is a flat muscle that sort of resembles a fillet of sole, and the Plantaris is a very small muscle that does not seem to provide any substantial function. The tendons of these three muscles come together to form the thick heel cord that is the source of many problems.
Unfortunately, as we age the healing process is not quite enough to support the constant pounding that the Achilles tendon receives. When an injury occurs, it is typically described as a feeling of being kicked in the back of the leg. Typically these tendons are injured during an explosive events such as jumping, landing or starting a "sprint". The typical age for this type of injury is between 40 and 50 years old and occurs predominantly in male patients. Up until recently, the recommendation was almost universally for surgical repair. The rationale behind this was to decrease the rate of rerupture. Now, with more advanced rehabilitation techniques, we are able to spare many people the pain of surgery. In the highly athletic population however, there is still the belief that surgical repair improves the strength and function in the long run. The recovery from any type of Achilles tendon rupture is quite long. It frequently takes 6-12 months to completely recover from such an injury and requires intensive rehab.
-J Fallon
-J Fallon
Tuesday, June 2, 2015
But I Don't Even Play Tennis!
Tennis elbow is a frustratingly annoying problem that is life's little "Welcome to Mid-Life!" gift. It has been referred to as some derivation of tennis elbow since the 1880's. The name came about not because it was believed to be caused by playing tennis, but because the physician that published essays in the 1880's about this problem noted that playing tennis seemed to make it more painful. Since then, the moniker has stuck. The true cause is usually quite variable: tapping sugar maples, crochet, working power lines... it rarely is directly caused by tennis. Ultimately, the problem is that you no longer heal faster than you are injuring yourself. What occurs is that the tendons that attach the extensor muscles of your wrist to the lateral part of your elbow sustain "Microtrauma" through your daily over-use (tapping maples trees as an example). In the ideal 18 year old elbow, this microtrauma would heal perfectly, without you noticing. Unfortunately, as we age, we are unable to heal as effectively and instead of healing with normal tendon, we form a less organized structure that vaguely resembles tendon. These microtrauma events pile up and eventually you end up with lateral epicondylitis, traditionally referred to as Tennis Elbow. There are literally hundreds of "treatments" for lateral epicondylitis. Like many other things in medicine (the common cold) if there are a bunch of remedies, nothing works for everyone.
Monday, May 11, 2015
Do I need an MRI before I see an Orthopedic Surgeon?
The short answer to this is no. Well, not usually. MRIs are a very useful tool in orthopedic surgery, and we have come to depend on them for many facets of diagnosis and surgical planning.
There is commonly the thought that obtaining an MRI before your visit will "Save a step" in getting you better. What I frequently tell patients is that "I treat people, not MRIs". What that means is that I am far more interested in what you have to say and what your knee feels like, than what an MRI can tell me about your knee. So, getting an MRI may be necessary at some point, but may not be necessary.
MRIs also come in different varieties and I order special MRI sequences depending on the question I want answered. For example, if I suspect a SLAP tear in a young pitcher I will order dye injected into the shoulder joint prior to the MRI, making it an MR arthrogram. I will also request that their arm be placed in a certain position. I will not typically ask for an MR arthrogam in a 50 year old carpenter with shoulder pain in which I suspect a rotator cuff tear. If a patient has had previous surgery, metallic anchors would make an MRI useless because the metal would interfere with the magnets and the picture would be blurry. In that case, a CAT scan with dye injected into the shoulder would be a more useful way to see the structure of the shoulder.
The final reason not to try to get an MRI before you see me is that most primary care doctors have difficulty convincing your insurance that they should pay for an MRI. Their staff has to argue and struggle with the insurance companies to get the MRI "pre-approved". Frequently, despite all of their efforts, the insurance companies feel that the MRI is not warranted. Our office, on the other hand has a near flawless record of getting these approved. Part of this is my wonderful staff and their familiarity with the nuances of MRI scheduling and part of it is that for better or worse, my recommendation as a specialist carries more weight with the insurance companies than your PCP. So, let us do the work for you and save yourself the aggravation.
- J. Fallon
There is commonly the thought that obtaining an MRI before your visit will "Save a step" in getting you better. What I frequently tell patients is that "I treat people, not MRIs". What that means is that I am far more interested in what you have to say and what your knee feels like, than what an MRI can tell me about your knee. So, getting an MRI may be necessary at some point, but may not be necessary.
MRIs also come in different varieties and I order special MRI sequences depending on the question I want answered. For example, if I suspect a SLAP tear in a young pitcher I will order dye injected into the shoulder joint prior to the MRI, making it an MR arthrogram. I will also request that their arm be placed in a certain position. I will not typically ask for an MR arthrogam in a 50 year old carpenter with shoulder pain in which I suspect a rotator cuff tear. If a patient has had previous surgery, metallic anchors would make an MRI useless because the metal would interfere with the magnets and the picture would be blurry. In that case, a CAT scan with dye injected into the shoulder would be a more useful way to see the structure of the shoulder.
The final reason not to try to get an MRI before you see me is that most primary care doctors have difficulty convincing your insurance that they should pay for an MRI. Their staff has to argue and struggle with the insurance companies to get the MRI "pre-approved". Frequently, despite all of their efforts, the insurance companies feel that the MRI is not warranted. Our office, on the other hand has a near flawless record of getting these approved. Part of this is my wonderful staff and their familiarity with the nuances of MRI scheduling and part of it is that for better or worse, my recommendation as a specialist carries more weight with the insurance companies than your PCP. So, let us do the work for you and save yourself the aggravation.
- J. Fallon
Sunday, May 10, 2015
What Kind of Music Do You Play in the Operating Room?
I was recently asked this by one of my high-school aged patients. My response was, "It depends... what do you want to listen to while I operate on you?". So we spent the next 45 minutes exploring the K-Pop station on Pandora.
I love music. I grew up playing the guitar (poorly) and I recently returned to learning the guitar (still struggling). I believe in the healing and soothing properties of music. I believe in the common language of a well done melody. There are some that believe that music is a distraction in the operating room and there is no place for it. I had a mentor the would reference the sound of the electronic heart monitor (a hopefully constant beep…beep... beep) as music to his ears and the only thing he wanted to listen to. While I respect him immensely and his perspective, in my OR music has a definite role. There are times for ultimate focus and silence, but the reality is that the OR is an inherently tense environment filled with people of diverse backgrounds that have to work together quickly, efficiently and precisely. Anything that we can do to decrease the anxiety and stress level, makes for a more effective team and better surgery. There was actually a study in the Journal of the American Medical Association that demonstrated improved relaxation and motor skills of surgeons listening to music of their choosing.
Some days require something mellow like Jack Johnson or Big Head Todd. Other days need a kick in the pants and we get Ja Rule. Most days end with AC/DC and you don’t want to hear my OR Jazz mix… that’s a bad day. Music is good for me, it is good for my team and it also good for the patient. Playing melodies for patients has been shown to decrease anxiety levels and heart rates in perioperative patients.
Fun fact: Apollo was the god of Music and Healing
Monday, May 4, 2015
The Biology of ACL Reconstruction and Regeneration
One of the best examples of the wonders of modern medicine is Anterior Cruciate Ligament reconstruction. Because the body is unable to heal the ACL on its own, it requires reconstruction in order to restore normal function to the knee. The process of ACL regeneration relies heavily on the biology of your knee.
When I reconstruct your ACL, I take a tendon, either from an organ donor or from a different part of your body, then place it where I want a ligament to grow. Your body uses this tendon as a scaffolding to regenerate a new anterior cruciate ligament. This process occurs and 3 phases. The initial phase is characterized by necrosis or cell death. During the first 4 weeks after surgery, your body tears down all of the living cells in the graft, leaving only nonliving tissue as a blueprint for the final ligament. The second portion of the regeneration process is called the proliferation phase. This usually occurs in the second and third month after surgery. This is characterized by influx in your own body’s cells into the remaining scaffolding. The scaffolding also undergoes changes that cause significant weakness in the graft. 6-8 weeks after surgery is typically thought of as the weakest point and the time where of the structure of the graft needs the most protection. The final phase, the ligamentization phase begins about 3 months after surgery. During this time, the graft is slowly and steadily getting stronger and becoming more like the original ACL. There is no clear end point however there is plenty of evidence suggesting that the graft will continue to mature over the following year.
When I reconstruct your ACL, I take a tendon, either from an organ donor or from a different part of your body, then place it where I want a ligament to grow. Your body uses this tendon as a scaffolding to regenerate a new anterior cruciate ligament. This process occurs and 3 phases. The initial phase is characterized by necrosis or cell death. During the first 4 weeks after surgery, your body tears down all of the living cells in the graft, leaving only nonliving tissue as a blueprint for the final ligament. The second portion of the regeneration process is called the proliferation phase. This usually occurs in the second and third month after surgery. This is characterized by influx in your own body’s cells into the remaining scaffolding. The scaffolding also undergoes changes that cause significant weakness in the graft. 6-8 weeks after surgery is typically thought of as the weakest point and the time where of the structure of the graft needs the most protection. The final phase, the ligamentization phase begins about 3 months after surgery. During this time, the graft is slowly and steadily getting stronger and becoming more like the original ACL. There is no clear end point however there is plenty of evidence suggesting that the graft will continue to mature over the following year.
Monday, April 13, 2015
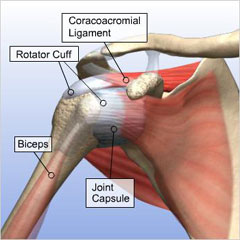
Will My Frozen Shoulder Ever Get Better?
Frozen shoulder, or Adhesive Capsulitis is a frustrating and painful condition that typically effect people in the 40's and 50's. It almost sneaks up on you, feeling like a tweaked shoulder from doing something dumb like trying to catch the soda can as it rolls off the counter. It can be a very painful process to go through, interrupting your sleep, your work and effecting pretty much every aspect of your life. Along with the pain comes an inability to move your shoulder.
The frustrating part of this is that it doesn't matter how high a pain threshold you have or how hard you work to stretch, you can't make this go away any faster. Beyond that, there is not much I, as your surgeon and physician can do about it either. It has a mind of it's own. Aggressive physical therapy, forceful manipulation, surgery all fail to make this go away any sooner. My role in getting you better is primarily supportive. I can offer you cortisone injections to help make the pain bearable. I can show you some stretches to help make you shoulder slightly more useful, but ultimatelly, frozen shoulder thaws on its own schedule. Even worse... it can take up to 2 years to go away. Ulitimately, it does resolve and you should expect full use of your arm in time.
For more information, you can read this handout from the Journal of Orthopaedic and Sports Physical Therapy or call our office for and appointment.
The frustrating part of this is that it doesn't matter how high a pain threshold you have or how hard you work to stretch, you can't make this go away any faster. Beyond that, there is not much I, as your surgeon and physician can do about it either. It has a mind of it's own. Aggressive physical therapy, forceful manipulation, surgery all fail to make this go away any sooner. My role in getting you better is primarily supportive. I can offer you cortisone injections to help make the pain bearable. I can show you some stretches to help make you shoulder slightly more useful, but ultimatelly, frozen shoulder thaws on its own schedule. Even worse... it can take up to 2 years to go away. Ulitimately, it does resolve and you should expect full use of your arm in time.
For more information, you can read this handout from the Journal of Orthopaedic and Sports Physical Therapy or call our office for and appointment.
Monday, April 6, 2015
Recovery from Knee Arthroscopy
A recent question came in asking about recovery from a "Knee Scope". Knee arthroscopies are one of the most common orthopedic procedures across the country, but it is important to keep in mind the the scope is only a tool, like a screw driver or a hammer. Much like a hammer, scopes can be used for a variety of reasons and the recovery is based on what was done to the knee. Most of the time, meniscal tears and loose bits of cartilage are trimmed.
In this instance, patients are encouraged to use the leg carefully, while the swelling and inflammation from the surgery quiets down. From there, it typically takes patients anywhere from 1-3 months to return to their "pre-surgery activity level". There are more involved surgeries that are done arthroscopically such as meniscal repairs, microfractures and cartilage transfers. These require slower and more involved rehabs. ACL reconstructions are also done arthroscopically, and these require a 6-12 month rehab. If you would like more info on my ACL rehab protocol, you can follow this link to our Patient Resources Page or The American Academy of Orthopedic Surgeons.
Sunday, March 29, 2015
The End of AT appreciation month...
As Athletic Trainer Appreciation Month comes to a close and the spring thaw begins, give it up for our local athletic trainers. They are doing great work keeping the Pioneer Valley an active and vibrant community! The people at Strides Human Performance, Energia Fitness, Advance Perfomance Player Development, Conca Sport and Fitness, Integrated Muscular Therapy and countless others are working crazy hours to get you back in the game...
Sunday, March 22, 2015
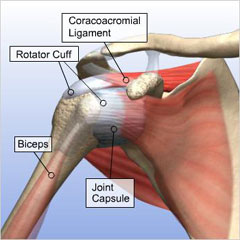
Can I golf after my Shoulder Replacement?
The rehab and recovery from a shoulder replacement is an arduous process but one that is usually quite rewarding. The technology and surgical techniques behind shoulder replacements have made huge advancement recently. And while they may not have you pitching for the Red Sox this summer, they can go a long way towards ridding you of constant shoulder pain and get you back on the links.
In a recent survey of shoulder surgeons in the Journal of Shoulder and Elbow Surgery, ~74% allowed their patient to return to some sort of sport with the majority recommending non-contact, low risk of fall sports. Many of my patient return in swimming, golf, cycling and even tennis after a shoulder replacement. To be fair, if you couldn't play the piano before you get your shoulder replaced, it is unlikely that you will be able to play afterwards.
In a recent survey of shoulder surgeons in the Journal of Shoulder and Elbow Surgery, ~74% allowed their patient to return to some sort of sport with the majority recommending non-contact, low risk of fall sports. Many of my patient return in swimming, golf, cycling and even tennis after a shoulder replacement. To be fair, if you couldn't play the piano before you get your shoulder replaced, it is unlikely that you will be able to play afterwards.
Wednesday, March 18, 2015
I am a 43 year old Athlete and I tore my ACL, now what?
The short answer is, you don't need it. As a sports medicine surgeon, I live to get people "back in the game", be that Eathampton HS football or the over 40 soccer leage at Allsports. However, most of life does not require an ACL. So why can I ski bumps without an ACL, but my kid's babysitter should have it reconstructed? The answer lies with age. In the over 40 population, it has long been thought that there are 3 groups of people who tear their ACLs: Copers, Adapters, and non-Copers.
If you are a Coper, with some dedicated rehab and a brace, you can return to all of the dumb things you were doing before you tore your ACL. If you are an Adapter, with some good rehab and a whiff of mortality, you get back to life and many of the things you were doing before, but you take a less aggressive approach to athletics. You limit the cutting, twisting, pivoting sports, but can remain active in athletics that are less "ACL Dependant". If you are a non-Coper, you knee feels unstable inspite of dedicated rehab and a brace, and you are unwilling to accept the limitations that this injury has foisted on you. In this case, there is decent evidence that an ACL reconstruction will help you stabilize your knee and get you "Back in the Game". For most middle aged athletes, life is busy and they don't have the time to jump right into the 6-9 month rehab that an ACL recontruction requires, so the most common recommendation is to try non-surgical management of the ACL tear and see how it goes.
If you are a Coper, with some dedicated rehab and a brace, you can return to all of the dumb things you were doing before you tore your ACL. If you are an Adapter, with some good rehab and a whiff of mortality, you get back to life and many of the things you were doing before, but you take a less aggressive approach to athletics. You limit the cutting, twisting, pivoting sports, but can remain active in athletics that are less "ACL Dependant". If you are a non-Coper, you knee feels unstable inspite of dedicated rehab and a brace, and you are unwilling to accept the limitations that this injury has foisted on you. In this case, there is decent evidence that an ACL reconstruction will help you stabilize your knee and get you "Back in the Game". For most middle aged athletes, life is busy and they don't have the time to jump right into the 6-9 month rehab that an ACL recontruction requires, so the most common recommendation is to try non-surgical management of the ACL tear and see how it goes.
Monday, March 9, 2015
Specialization in Youth Sports
I have many families asking about young kids "specializing" in one sport. There is a perception that kids need to master specific skills if they are to continue to compete. Below is an interesting take on the growing specialization of athletic kids.
"As more and more kids play the same sport year-round from an early age, they are increasingly vulnerable to injury. A report this year by the sports medicine department at Loyola University of Chicago found that "kids are twice as likely to get hurt if they play just one sport as those who play multiple sports."" Link to the complete Daily Herald article
Saturday, February 21, 2015
Baseball injury prevention for kids
Truck day has come and gone! Pitchers and catchers have reported to spring training. Youth baseball is soon to follow. With this in mind, here is a link to some important information about keeping your throwers healthy. Overuse injury prevention tips
Friday, February 20, 2015
Computer and Phone systems back on-line
Thank you for all of your patience. We apologize for any inconvenience. If you have any questions, please call us!
Wednesday, February 18, 2015
Computer and Phone systems down
***Please be aware that our telephones and computers are currently down. If you have a medical emergency please call 911 or go to your nearest emergency department. We apologize for this inconvenience and hope to have our systems up and running again shortly***